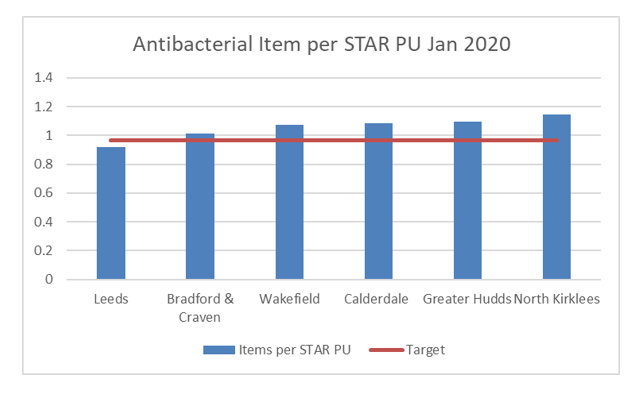
High levels of antibiotic prescribing have long been an issue in Calderdale and for most of West Yorkshire, with prescribing above target in many of the West Yorkshire CCGs, and resistant infections occurring all too regularly - including cases of multi resistant infections.
In England, to account for differences in the age and gender profiles of patients that may explain legitimate variation between practices, comparisons of antibiotic prescribing rates are typically performed by evaluating antibiotic use per Specific Therapeutic group Age-sex weighting Related Prescribing Unit (STAR-PU).
In December 2020, just pre-pandemic, the below chart shows the picture across West Yorkshire. Only Leeds was below the nationally set target which was 0.965 items per STAR PU at that time. Calderdale was in the worst 15% nationally for total antibiotic prescribing, meaning that Greater Huddersfield and North Kirklees were also, by default, in the worst 15% and Wakefield was in the worst quartile. Data downloaded from ePACT2.
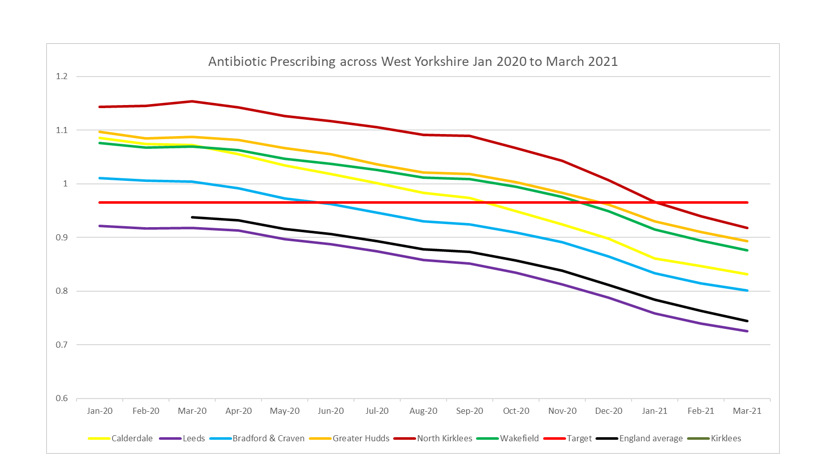
Due largely to the pandemic, antibiotic prescribing nationally dropped – quite significantly - in 2020 and right through to March 2021. All 6 CCGs in West Yorkshire dropped, closely following the national pattern in most cases.
In Calderdale, data is shared with member practices quarterly. Unfortunately, there may have been some unintended consequences of sharing the data. When we shared data with clinicians in our member practices the drop in prescribing was seen as a good news story… antibiotic prescribing had dropped, the CCG was now (significantly) below the target, the clinicians were doing well, Calderdale was dropping faster than other CCGs and was no longer in the worst quartile of prescribers.
In my opinion this may have meant clinicians allowed Antimicrobial Stewardship (AMS) to drop down the agenda. In light of everything that was going on (and indeed is still going on) in primary care, this is perhaps understandable, but worrying, nevertheless.
All of the above was of course true - it just didn’t reflect the full picture. The fuller picture would have included that despite being well under the target at that time, Calderdale and some of the other CCGs in West Yorkshire were still in or only just outside the worst quartile for prescribing of antibiotics, so amongst the highest prescribers in the country.
Again, due in large to the pandemic and the changes made to how patients are seen in primary care, it was noted locally by some of our clinicians that they recognised that remote prescribing of empirical antibiotics was increasing significantly. This was fed back in Autumn of 2020 - initially just anecdotally and then more widely during a meeting held in Calderdale to discuss the risks of remote antibiotic prescribing. One clinician noted it was evident already in practice that antibiotic prescribing was going up - if the clinician had a phone consultation or video consultation and the patient sounded borderline in terms of whether an antibiotic was indicated, they would be more inclined to give a prescription to safety net than perhaps they would if they were in a face-to-face consultation.
If we couple together these issues – high prescribing levels of antibiotics pre-pandemic, different ways of working as a result of the pandemic and a lower threshold for prescribing empirical antibiotics when consulting remotely - it means there is an increased risk that patients may be prescribed antibiotics inappropriately as a result. There could also be a longer term risk that patients get used to having prescriptions for antibiotics issued remotely, which could cause problems in the future in terms of their expectations changing and potentially increased demand.
Prior to the pandemic approximately 80% of consultations were done face to face. During the early stages of the pandemic in March 2020, NHS England advised all GPs to move to total triage and remote consultations (consultations by telephone, video or online). Patients were still seen face to face if needed, as they have throughout the pandemic, but many were dealt with remotely in entirety. This meant physical examinations were difficult to do routinely which may have led to over prescribing of empirical antibiotics. Indeed, during the early stages of the pandemic when appointment numbers did go down it may be that, despite the numbers of antibiotic items per star PU falling according to the data as seen above, the actual numbers of antibiotic items per appointment given was higher2. The changes in how patients are seen are becoming more permanent with many practices still using total triage – so there is an ongoing risk.
The situation now:
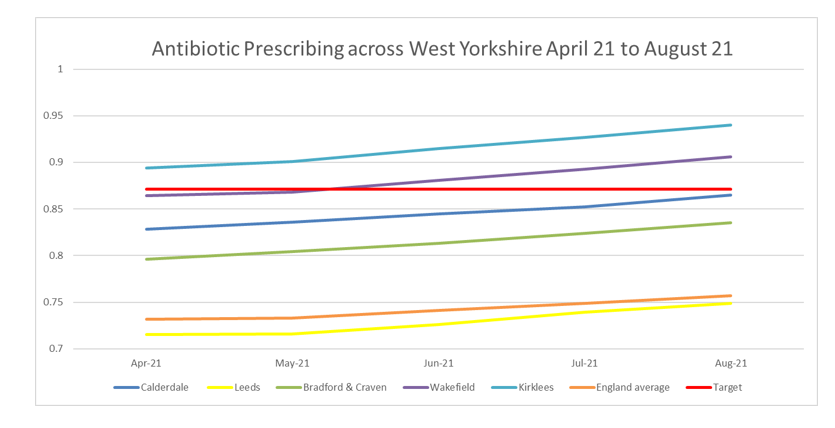
On 23 September 2021 NHS England released a letter announcing that the Antibiotic prescribing target had been reduced, from 0.965 items/STAR PU to 0.871 items/STAR PU. The target for primary care antibiotic prescribing had been adjusted in 2021-22 to align it with the UK AMR National Action Plan ambition to reduce community antibiotic prescribing by 25% by 2024.
This reduction in target, coupled with antibiotic rates increasing across West Yorkshire and nationally since May 2021, mean that two of the CCGs in West Yorkshire are already above the new target and a third is only just below the target.
This latest data shows a very different picture than the one seen during the pandemic, and it shows the need for a focus on Antimicrobial stewardship in primary care once again.
How can we improve?
In the meeting in October 2020 about remote prescribing of antibiotics, a number of themes were identified by the clinicians attending the meeting as being a potential issue and some possible mitigations to some of the risks.
Overarching issue: Antibiotics are being issued , potentially too readily, due to consulting with patients remotely.
Guidance: Clinicians are not always thinking about probabilities of infection being bacterial and not always thinking about current guidance during the consultations. Audits at one local provider shows clinicians are not following or aware of latest guidance e.g., routinely giving antibiotics for sinusitis when patients have not had symptoms for 10 days and in one CCG an audit showed 80% of patients were getting the wrong antibiotic for sinusitis.
-
Suggest practices include a link to current guidance in favourites rather than downloading a copy to desktop, so guidance stays current. In one CCG it was noted some practices were still referencing very old antibiotic guidance which has been saved to the PC.
-
Produce a summary of the most common infections and current treatment (see below).
-
Note the best way to reach people is regular messaging - short and sweet. Weekly/key messages often too much information for clinicians to absorb quickly.
Examinations: not possible in many remote consultations, and the onus has been on not seeing patients unless necessary. Cannot always diagnose with certainty and can’t always determine the severity.
-
Clinicians can get patients to provide photo of otitis externa or tonsils, or to take a urine sample and describe it – e.g. whether it is cloudy. This all helps with building the picture.
Repeat prescriptions of antibiotics: for example COPD rescue packs on repeat can be difficult not to issue.
-
All antibiotics should only be on repeat if necessary and reviewed regularly.
-
Consider steroids only in COPD exacerbations unless there are infection markers.
-
Consider involving the community respiratory team if COPD patients exacerbating very frequently.
Patient Education: it can be difficult for patients to accept that there is no need for a prescription when they feel ill.
-
Utilise patient education resources such as delayed prescription pads, available at the recently updated Target website: https://elearning.rcgp.org.uk/course/view.php?id=553
In response to some of the mitigations noted in the meeting and to support the AMS agenda in primary care in these difficult times, Calderdale CCG and the South West Yorkshire APC have produced a local summary of the most common infections. You can download this here.